Abstract
Background
Sickle cell disease (SCD) is characterized by hemoglobin polymerization leading to vaso-occlusion, chronic hemolysis and vasculopathy. Parvovirus B19 (B19) infection causes an acute arrest of erythropoiesis leading to reticulocytopenia and potentially life-threatening anemia in patients with chronic hemolysis such as SCD. Diagnosis of B19 infection relies on clinical history in combination with expensive and often belated serological and molecular testing. The immature reticulocyte fraction (IRF) is a relatively new reticulocyte parameter available on automated hematology analyzers that assesses the maturity of circulating reticulocytes by quantifying the fraction that stain strongest for RNA.
Aims
We hypothesized that the IRF could provide diagnostic information in the evaluation and management of patients with SCD who are being evaluated for B19 infection. Specifically, given that the IRF quantifies the fraction of circulating reticulocytes that have just exited the bone marrow and are least mature, we speculated that changes in IRF would precede changes seen in the reticulocyte counts in aplastic crisis and recovery.
Methods
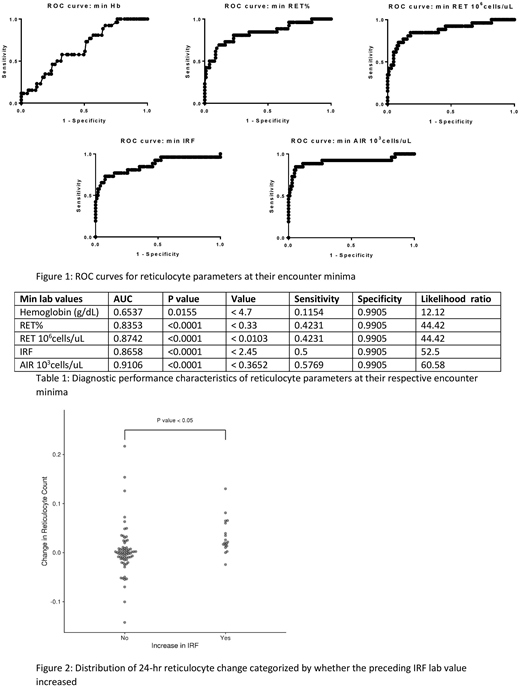
We performed a retrospective analysis of records at the Children's Hospital of Philadelphia of complete blood count (CBC) and reticulocyte indices in patients with sickle cell disease in whom B19 infection by PCR testing was assessed between January 1, 2015 and October 31, 2017. CBC testing was performed on the Sysmex XN 3000 analyzer. Medical records were reviewed to verify that the B19 testing was sent during an acute aplastic episode. Diagnostic performance of reticulocyte percent (RET%) and count (RET) compared to the IRF and the absolute IRF count (AIR) was assessed by receiver-operator characters (ROC) curves on GraphPad Prism. For recovery studies, an increasing IRF was defined as an increase of 10 per 24 hour period and a recovering reticulocyte count was defined as an increase of 50,000 cells/uL per 24 hour period.
Results
At baseline, patients with SCD have an average IRF of 27.2% (16.7 - 37.7%), far higher than the reference interval (9.3 - 17.4%). This parallels the elevations in reticulocyte counts in this population and relates to their chronically high RBC turnover. A total of 119 patients had B19 testing performed in the study period of which 26 were found to have acute infection. The most common diagnoses amongst the B19 negative patients were unspecified fever/viral syndrome, vaso-occlusion/pain crisis, and acute chest syndrome. ROC curve analysis demonstrates that RET%, RET, IRF, and AIR lab values are predictive of B19 infection on the day that B19 PCR testing was sent with an AUC of 0.73, 0.76, 0.76, and 0.83 (p < 0.001 for all) respectively. The AUC for each parameter increased when the respective minimum value was analyzed; RET%, RET, IRF, and AIR showed an AUC of 0.83, 0.87, 0.87, and 0.91 (p < 0.0001 for all, figure 1 and table 1). In particular, an IRF value below 2.45% demonstrated a sensitivity of 50% and a specificity of 99% for B19 infection in the study population. Finally, amongst B19 positive patients we found that an increasing IRF was strongly associated with a reticulocyte recovery within the following 48 hour period (chi-square p-value = 0.015). A rising IRF was associated with a higher mean reticulocyte increase in the following assessment (2,500/24 hour period vs. 33,000/24 hour period, p < 0.05, figure 2). Moreover, an increasing IRF had a sensitivity of 31% and a specificity of 92% for a recovery in reticulocyte count. These results were consistent amongst all aplastic patients who were tested for B19 as well (data not shown). These data suggest that a high IRF is closely associated with a rising reticulocyte count within the following 24-48 hours.
Conclusions
Our data confirms that amongst a cohort of complicated patients with SCD and other causes for reticulocytopenia, the IRF is highly specific for detecting the severe aplasia caused by B19 infection in this group. This additional data may be useful in better triaging patients with SCD and reticulocytopenia and potentially in improving utilization of the more expensive B19 diagnostic testing. Furthermore our study suggests that an increasing IRF predicts reticulocyte recovery in reticulocytopenic patients with SCD and could have utility in clinical decision making such as whether to transfuse packed red blood cells or whether they can be safely discharged from the hospital.
Lambert:Amgen: Membership on an entity's Board of Directors or advisory committees; Sysmex: Consultancy; Bayer: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees; Educational Concepts in Medicine: Consultancy; Summus: Consultancy; Rigel: Consultancy; Shionogi: Consultancy; CSL: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal